Wound care is not just a scleroderma thing. I was recently at a social gathering and was summoned to a conversation about wound care. This is what we talked about.
Short video: here. Below are some suggestions and links.
Not a Doctor
I am not a doctor and have no medical training. I am sharing anecdotal stories about what has or has not worked for me. For medical advice, please get in touch with your physician.
When in Rome, do as the Romans do.
It’s tough to explain the evolution of wounds. When I call the nurse line at the VA to ask advise, nurses easily walk me through my description. In my doctor’s office, I have less time. And yes, they can see my wounds, but sometimes things happen and go away before I see a doctor. I try to take pictures. They are great for reference. Being able to use terms helps.
Here’s what being Roman did for me:
- It made me a better communicator. Going in, knowing how to describe my symptoms, or being able to name which knuckle is infected by using proper labels for joints can save time.
- It also made me a better listener. Listening carefully and looking for medical terms helps me stay calm. It helps me process things better when I feel emotionally overwhelmed—that takes practice.
- Decreased confusion: I once referred to a shoulder muscle that starts with an “L” as my labia. Not the best conversation on my speakerphone at Applebee’s.
Wound Cleaning
When it’s time to clean my wound, I use baby shampoo, or a spray recommended or prescribed by my wound care specialist. I use a non-snagging gauze and pat the wound dry.
To Debride or Not to Debride?
Now there’s a shitty question. Debridement (duh·breed·muhnt) is almost as fun as shoving thumbtacks under my nails. Debridement is usually the surgical removal of lacerated, devitalized, or contaminated tissue. (Devitalized is just a pretty word for dead.)
By surgical, they mean a procedure done in a doctor’s office. I am wide awake for mine, and the only thing used to numb is liquid lidocaine. It’s as weak as it sounds. Wound debridement is very painful. When I had calcinosis in my leg for one year, I saw a good wound care specialist, it decreased my overall pain after every visit.
With scleroderma and other vascular degenerative conditions, chunks of skin die. These small chunks are not rotted; they become dead skin and fall off. But if deep, they can snag and cause pain. I learned at a very early time in my illness that when that happens, I need to finish the job. Before I knew about wound care specialists, I did what I like to call “Home Surgery.” Do not try this at home.
Is Debridement Painful?
No, it’s mother fucking painful. My pain level sometimes feels like an 11 during debridement, but it quickly disappears once it’s over. Sometimes, I’m sore afterward, or I need a nap after the adrenaline high, or apologies all around the room for my foul language.
Avoid Medical Mayhem
I’ve had wounds on my hands for a few weeks now. Debridement on my hands is extremely painful compared to when I had wound care on my leg. At this last wound care appointment, a nurse tried to pack my wound with Prisma. I asked her not to because all I could think about was the pain I felt when I removed my Prisma bandages. Well, the joke is on me. When removing the Prisma, if I add water, it breaks down like cotton candy and removes easily. But even the thought of pain can sometimes cloud my judgement.
The problem was that my wound needed to be packed with Prisma in order to heal properly, but by refusing it, I made it worse. When I took off my bandage that night, I had a nice layer of biofilm. Beneath that was some lovely yellow puss. Even after soaking, devitalized cells stayed attached, and now I have to see my wound care specialists re-scrape it. My lesson: When my doctor tells me to pack my wounds, do as she says. I delayed my healing by one week.
Back to Wound Care
It is important to see a doctor anytime there is an unhealing wound. If you are unable to see a wound care physician right away due to consult issues or insurance delays, here is a list of supplies I use for difficult-to-manage wounds. Everything I link here is covered by Medicare, except for coban & baby shampoo.
1. Baby shampoo: to clean my wounds. I dab a drop or two of baby shampoo on a wet cotton ball , or non-snagging gauze or gently clean with my fingers and rinse.
2. Silicone Foam Dressing : It’s great for wounds that will ooze and wounds that don’t. It also sticks to the wound without hurting when removed. I cut it into pieces for small wounds. Usually, I use an antimicrobial silver wound dressing.
3. Gauze Pads: I am addicted to Band-Aid brand non-stick gauze. It’s the most bang for my buck and provides an absorbant cousion over my wounds. I use these instead of silicone foam dressing sometimes.
4. Wound retention tape: It sticks almost anywhere, removes without taking skin with it, and doesn’t iritate my skin.
5. Coban: It’s like an Ace bandage that sticks to itself. Great for when low on tape or provide extra protection. Caution, Coban should be wrapped loosely. Its use is mainly for comression, but can be made loose by stretching and wrapping loosely. I get the 1″ or 2″. It’s easier to apply.
The best way to learn to use it is with instruction from your wound care specialist and then following their directions. When I wait to see my wound care specialist, I use those supplies to keep it from getting even worse. It can seem like a lot, but that extra time spent protecting can speed up healing time and reduce chance of infection.
Good luck, and if you’d like to share your experience, please do in the comments.
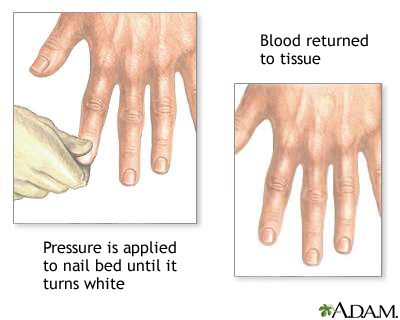
I don’t really remember my first Raynauds attack, but I remember the first time I saw it happen. In 1993, during the last year of my enlistment in the Navy, I had shore duty. Four nights a week, I attended EMT school at Miramar College. I was a “patient” for someone to practice leg splinting. After splinting, blood flow is checked by something called capillary refill.
Capillary refill tests the speed of blood return to a spot on our bodies- usually fingers and toes. When pinched, blood will disappear but should immediately return. In my case, my toenail remained white longer than it should have. Slow blood return is a symptom that indicates something is wrong. My big toe had a slow blood return and while the student EMT was checking the device, my toe turned blue.
The instructor came by to help us troubleshoot. She asked if I was diabetic. I was not. She advised me to get it checked. What she didn’t know is that I had been experiencing numbness and tingling in my fingers and toes with the smallest temperature drop for a little over a year.
I had already been seen by two rheumatologists at Balboa Navy Hospital and my blood tests were inconclusive. I was advised to stop smoking and stop taking birth control pills. I quit smoking and stopped taking the pill, but it kept happening When I followed up with my rheumatologists, they said it was probably nothing and just the way my body works.
The following October, I was seated on the examination table at the Madison Wisconsin Veterans Hospital. Two more rheumatologists were examining me. They looked through a jeweler’s loop just like the rheumatologists at Balboa did, but this time they had an immediate answer; scleroderma.
I was stunned. I had never heard of scleroderma, and neither did my boyfriend who drove me to the doctor that day. My first question was, “Will it kill me?”
Other than the name of my diagnosis, the rheumatologists had very little information about scleroderma and how it would effect me. I was told it could kill me in three years, or I could live to be one hundred.
My boyfriend said that I shouldn’t be consumed by whether or not scleroderma killing me, because I could waste all of my time worrying and end up getting killed by a bus instead. Great, not I’m scared of scleroderma and buses. But kidding aside, he had a point. Nothing had changed since walking into the doctor’s office, except I had a name for what was causing my fingers and toes to turn blue.
Twenty-seven years later, I am grateful to my ex-boyfriend for that perspective. It shaped my way of thinking more than I could’ve imagined back then. My only regret about that day is that I didn’t ask, “Can I drink with these meds?”