We all have a friend who starts talking about something and then takes us somewhere we had no idea we were going. It’s me. Hi, I’m Karen. This post is all over the place and I’m taking suggestions.
My goal with the blog and now my podcast- I have yet to update – is to bring chronic illness awareness outside the scleroderma community, but there’s more to it. After twenty-seven years, I finally understand why I am so pissed off about American Healthcare. American Healthcare is the problem.
Since being diagnosed with my second chronic illness, I realized scleroderma was only one of my issues. It’s never just scleroderma.
But first, scleroderma. Like many with chronic illnesses, I felt isolated because I knew no one else with scleroderma when I was diagnosed. I used to get upset when friends and family went to cancer fundraisers, but never my scleroderma walks.
It’s not that they didn’t like me. It’s that scleroderma had never touched their lives on a daily basis like their loved one with cancer or whatever wasn’t scleroderma. So I began to look for things I have in common with other people or illnesses. The one thing I found constant in everyone is that we all face challenges. One challenge is not more valid than another. It’s not a contest. Also, when there are breakthroughs in conditions or diseases other than mine, this elevates care for all.
Everyone knows about cancer. But did you know that cancer medications like Ofev for lung cancer treat pulmonary fibrosis in scleroderma? Do you know how they found out? Because when a drug is developed and approved by the FDA, the research doesn’t stop there. It continues. Things change as more information is studied, and then studies are studied and repeated.
I have pulmonary fibrosis due to scleroderma. The good news is that in the research of medication to treat lung cancer, someone noticed some benefits for individuals with pulmonary fibrosis. Recently, that medication was approved to treat and prevent pulmonary fibrosis with scleroderma by the FDA.
The situation I faced was not unlike what all Americans faced during the COVID vaccine roll-out. Is the benefit worth the risk?
Now, like the covid vaccine, Ofev is relatively new. Both medications were not created overnight. Although it felt like it with the covid vaccine, it was not created overnight. Here’s why: In my case, I had my radar up because I knew that someday my lungs would harden enough for me to need supplemental oxygen or a lung transplant. So when my prescribing physician told me the FDA approved something for pulmonary fibrosis with scleroderma, I wanted it yesterday.
With the Covid vaccine, there were already vaccines available for the viruses like Covid. Once we were able to genetically code it (and by we, I mean researchers doing actual research. not blog comparison), it was tested, approved, and tested more and then approved for the population by the FDA. No one pulled this vaccine out of their ass. Just like no one pulled Ofev out of their ass.
With Ofev, the side effects and complications risks were present, and I had to learn how to manage them so my body could continue to tolerate prolonged use. Was I going to try it, even though it’s relatively new but has been deemed safe by the FDA? Fuck yes. Because I am lucky to have lived long enough to stop the hardening of my lungs.
The risk of side effects and even death, is worth it to avoid more hardening of my lungs. This is an opportunity to keep my lungs functioning without supplemental oxygen or the need for a lung transplant.
So if you come at me with the whole, Covid vaccine is new, and you’re declining your vaccination because some guy with no medical training tells you it’s not studied enough, I will have to tell you to fuck yourself. That’s how medicine works, asshole.
Those who refuse to get vaccinated for anything that benefits public health (if your health allows you to be vaccinated), you put millions of other Americans, including me, at risk of dying. Due to the way medical necessities are handled in the United States, many freedoms are already taken away from disabled and chronically ill Americans.
So we’re restricted by the shitty American healthcare system, and then there are self-righteous anti-vaxxers restricting us even more.
We already receive the bare minimum of assistance that helps us thrive in our community. We are at the mercy of our caregivers, the for-profit companies that pay shareholders instead of staffing best for patients. We are forced to wait for life-sustaining care or given equipment that crates more problems because everything is cost over convenience.
I honestly don’t know my mission for this blog yet. But I know that Americans with disabilities and chronic illnesses are treated like shit here in the United States. And I’m fucking tired of it. Non-profit foundations compete for funds. Every year chronic illness patients have to travel to the capital of our nation and beg our representatives to help us get better research and care. Every time I see it, I admire the struggle these patients have to go through so whatever representative can have a photo opp saying, “See, I do care.” And then the same representatives vote against assistance programs after the photo opp. I am tired of seeing chronic illness patients and disabled Americans struggle needlessly.
I’m trying to figure out a way to show Americans who believe that Social Security and Medicare should be removed. That is a stupid idea. We need to make it better. And recent COLA increases are a start. When someone’s evaluated, it’s like a guilty until proven innocent thing. It isn’t enough to have the diagnosis; we must live at the lowest rung of the economic ladder.
I am lucky. I have veterans benefits in addition to Social Security and Medicare. People have told me that I should get the best because I’m a veteran. But you know, everyone who serves their country knows someone who has to choose between medicine, food, and rent. All Americans deserve the best healthcare. The reason we all don’t have it is because insurance companies can afford to pay lobbyists to keep it that way. It’s probably more complicated, but can we all start thinking about this?
The only suggestion I have right now is to look at who you’re voting for.
Hello! It’s been a while since I’ve posted, and I’ll catch you all up, but first, I see a lot of new readers so here is a little backstory. Those of you returning, welcome back! If you’d like to, skip the backstory, scroll down to Medical Mayhem.
In 1994, I was diagnosed with scleroderma, then in 2007 with sarcoidosis- that’s when I discovered chronic illnesses are just like potato chips: you’re going to have more than one.
After some harrowing infections, hospital stays, and new complications, I learned that if I could live through the worst of a complication, whatever I am going through is worth the fight because of what awaits me on the other side: More time with friends and family.
I have never called my diagnosis terminal. There have been some close calls and a few scares- not all related to my chronic illnesses. There are so many other ways to die.
Through the years, I learned to advocate for myself using humor. It started out by learning to explain scleroderma without making people cry. Today, most people I run into have heard of scleroderma thanks to Bob Saget and his work raising awareness and funds for a cure for the Scleroderma Research Foundation. But back in 1994, most people hadn’t heard of it, and those who did know, only knew of it as a death sentence. I am living proof that better treatments become available with time.
When my hands began to change, people asked more questions. I found that if I could bring in some humor, it kept people focused on what scleroderma was, instead of pitying me. Eventually, I used humor to teach doctors, nurses and anyone whomever would listen, about scleroderma.
I also have a little privilege as a veteran. Most people with scleroderma & sarcoidosis did not serve in the military. I did, and I have some badass benefits. I never have to choose between rent, medication or food like most people on Medicare and Social Security Disability. I have experience with private insurance before and after preexisting conditions were denied care, in addition to Medicare and Veterans healthcare.
I had health insurance from 2000 to 2008, used with my VA benefits. My current care is provided for free, and the rest of my life is through the VA. Now, instead of health insurance, I use Medicare to supplement my veterans care. My scleroderma & sarcoidosis expert is not part of the VA, so I use medicare to see him. He then prescribes medication and treatment. The rheumatologists at the VA and my outside specialists work together as a team.
Every veteran’s hospital is connected to a medical school which makes them teaching hospitals. My VA hospital works with UCLA, and my outside specialist is a UCLA faculty member. So my doctors from the VA have a relationship with my scleroderma specialist.
Medical Mayhem
I have been told many times by people with different experiences than mine that VAs should be privatized or they are not as good as private hospitals. Not every hospital is equal; however, VA healthcare makes as many mistakes as private healthcare.
As far as mistakes, the ONLY difference between VA Healthcare and private healthcare is a public relations budget. Insurance paid facilities with companies like United Healthcare, Kaiser, or Blue Shield, well we’re going to hear more about “thriving” than all of those mishaps and mistakes thanks to a giant advertising and PR budget. So when something goes wrong at the VA, we only hear about that.
Here is how the clinics at my VA are set up: A doctor who is learning a specialty by practicing is called a fellow. Fellowes are supervised by attending physicians, who are practicing physicians and members of UCLA Faculty. Fellowes see the patients, assess them and bring in the attending physician at the end of the appointment.
Every time I work with a new fellow, they assess me. I listen to what they have to say, and if it conflicts with past treatment, I kindly explain to them how my care works.
For example, I met one fellow who would not prescribe opiates to anyone. She was very new to rheumatology. Anyone who’s ever asked for an opioid, knows what it’s like to be viewed as a drug addict. So when I explained how sometimes I need to “reset” my pain levels by taking Norco for one day or two, then add motrin and tylenol and titrate down to zero. In other words, I need a fucking break.
Pain is part of aging. People with chronic illnesses just experience pain at a younger age and at level eleven. Even after explaining I’ve been doing this for 27 years, and it’s in my chart, she still refused to prescribe them. It used to make me very upset, but with time, I learned that when I don’t agree with a fellow, I wait to speak to the attending. I asked the fellow to speak to her attending about it.
I went home from my appointment with Norco. My “secret” is that I have been managing pain for twenty-seven years. I know the value of Tylenol and Motrin, and I know from experience at what pain level I need a break to rest without any pain, and then I’m good. The attending physicians I have been working with for years know this.
I get that being new to a chronic illness and reading that even after twenty-seven years, I would still need to teach doctors about it doesn’t sound very reassuring, but it isn’t to me. I feel like every doctor, nurse, and medical provider I can teach about my issues, will help future scleroderma patients.
There is no cure for most chronic illnesses, but I have benefitted from new treatments exponentially for the last three decades. If someone else is diagnosed with scleroderma today with my symptoms, they will avoid damage and complications I had. I’m no saint, it does suck, but the opportunity to help others with my experience is fulfilling. It helps me power through things and gives me hope that I will continue to lead a long and fulfilling life.
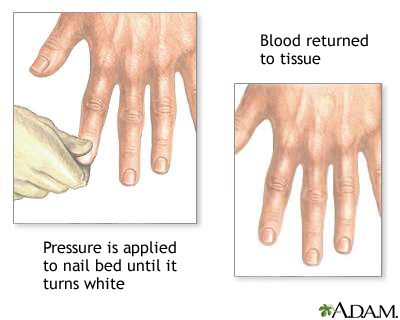
I don’t really remember my first Raynauds attack, but I remember the first time I saw it happen. In 1993, during the last year of my enlistment in the Navy, I had shore duty. Four nights a week, I attended EMT school at Miramar College. I was a “patient” for someone to practice leg splinting. After splinting, blood flow is checked by something called capillary refill.
Capillary refill tests the speed of blood return to a spot on our bodies- usually fingers and toes. When pinched, blood will disappear but should immediately return. In my case, my toenail remained white longer than it should have. Slow blood return is a symptom that indicates something is wrong. My big toe had a slow blood return and while the student EMT was checking the device, my toe turned blue.
The instructor came by to help us troubleshoot. She asked if I was diabetic. I was not. She advised me to get it checked. What she didn’t know is that I had been experiencing numbness and tingling in my fingers and toes with the smallest temperature drop for a little over a year.
I had already been seen by two rheumatologists at Balboa Navy Hospital and my blood tests were inconclusive. I was advised to stop smoking and stop taking birth control pills. I quit smoking and stopped taking the pill, but it kept happening When I followed up with my rheumatologists, they said it was probably nothing and just the way my body works.
The following October, I was seated on the examination table at the Madison Wisconsin Veterans Hospital. Two more rheumatologists were examining me. They looked through a jeweler’s loop just like the rheumatologists at Balboa did, but this time they had an immediate answer; scleroderma.
I was stunned. I had never heard of scleroderma, and neither did my boyfriend who drove me to the doctor that day. My first question was, “Will it kill me?”
Other than the name of my diagnosis, the rheumatologists had very little information about scleroderma and how it would effect me. I was told it could kill me in three years, or I could live to be one hundred.
My boyfriend said that I shouldn’t be consumed by whether or not scleroderma killing me, because I could waste all of my time worrying and end up getting killed by a bus instead. Great, not I’m scared of scleroderma and buses. But kidding aside, he had a point. Nothing had changed since walking into the doctor’s office, except I had a name for what was causing my fingers and toes to turn blue.
Twenty-seven years later, I am grateful to my ex-boyfriend for that perspective. It shaped my way of thinking more than I could’ve imagined back then. My only regret about that day is that I didn’t ask, “Can I drink with these meds?”



Hello! So…someone from a private healthcare referral service received someone else’s death notification from the VA, then reached out to Angela*, my home occupational therapy provider, and told her I had died. The good news is, I’m not dead. Like all my posts, this is another story about my personal experience that I hope will make us all better health care advocates for ourselves and others.
The VA Did Not Fuck Up
Whenever I talk about a medical mistake, it’s usually assumed that it’s a mistake by Veterans Healthcare. The VA did set me up with OT, but they did not call and notify anyone that I was dead. The VA informed Bob, an employee of a government contractor that refers VA patients to private health care providers about a death. Bob mistakenly thought the decedent was me.
How Did I Get Here? Dancing.
During a hospital stay in December 2021, Madison, my in-patient social worker concluded that I needed ongoing home occupational therapy. Madison had to send that referral to another department to determine if I am entitled to home occupational therapy. Once approved, my referral was sent to Bob’s referral service to connect me with an OT provider.
The provider sent a patient treatment manager, an OT named Emma, to determine the course of my treatment. Emma submitted the treatment plan, then another OT named Angela performed my treatment. In my case, I was approved for 10 visits, with a treatment plan of two visits per week, to be reassessed by Emma after all 10 visits.
I was frustrated that I would have to be reassessed every five weeks to determine that I had not somehow been miraculously cured. Through the years, I’ve had different partners but it’s always the same dance. Before I knew the dance, most practitioners dismissed my request for any type of preventive therapy for scleroderma. Before it became the public norm to encourage people with disabilities due to chronic illness to stay active, any occupational therapy to slow down the progression was considered a waste of money. It took a long time for me to find medical providers who would help and encourage me to live a fulfilling life that met my standards.
More for Context
It’s not that I would need OT twice a week forever. My goal is always to get to a spot where I need fewer visits. Why do I think that’s helpful? That’s how it was done in the second half of the 1990s for me through the Madison Wisconsin Veterans Healthcare System. Ever hear the phrase, “If you’ve ever been to one VA hospital, you’ve been to only one VA hospital”? It’s fucking mind-numbing how each state can have different policies for its VA healthcare system.
When I lived in LaCrosse, Wisconsin, I was allowed weekly occupational therapy at a private facility. Back then it was called Fee Basis, and it was god damn spectacular.
When I returned to California in 1999, I presented Debbie, the occupational therapist at the San Diego VA, my treatment plan from the Madison VA hospital in Wisconsin. Debbie determined that the cost of local OT therapy was a waste of government funds to delay the inevitable. San Diego and Loma Linda VA Healthcare System felt the same way. Now, I’m at the West LA VA and after fighting for decades, I’ve got the OT I need. Well, I did until my case was closed thanks to the death fuck-up.
Treatment Interrupted
When any kind of treatment or therapy suddenly stops, it sets me back in function and reduces the odds of my fingers recovering as well as they could have. It’s a domino effect. I subconsciously guard an injured spot only to become aware of it after getting an additional impact wound because I zigged when I should’ve zagged. Those injuries are painful and protecting wounds by compensating in other ways leads to additional injuries and infections. Once this domino effect is in motion, it’s as easy to handle as nailing Jello to a tree.
How I Dropped Off the Radar This Time
It’s easy to fall between the cracks when care suddenly stops. Frustration is overwhelming and there’s always a chance of a visit from the Crippling Depression Fairy. It’s happened to me a lot.
Here’s what happened this time. A couple of Fridays ago, my OT therapist Angela, tested positive for COVID. (I tested negative BTW) She had no symptoms, but my visits had to be canceled until Angela was cleared. They couldn’t just send out another because I had been exposed to Covid. A week went by, so I reached out to her via text to see if she had been cleared. That’s how I discovered my death had been reported.
Now, I’m into the second week of no treatment. I have yet to learn if the referral dance I mentioned earlier must start again. It could be one week or two, maybe a month.
So who is to blame? Is it VA Healthcare? Or the companies paid to manage my case? It’s neither and it’s both. This cluster-fuckery is baked into the design of our shoestring healthcare infrastructure. Screw-ups remotely related to VA services make it easy for public opinion to favor private health care over government-funded healthcare like the VA. If funded properly, VA Healthcare could potentially make a good model for universal healthcare or Medicare for all. But we can’t have that. A small percentage of Americans need to collect dividends for their big pharma and health Insurance stock in addition to those “life saving” stock buybacks.
Ever notice that screw-ups at VA hospitals are all over the news, but rarely from our private hospitals? That’s because private health insurance and private hospitals have bigger public relations budgets.
If government-funded healthcare like VA healthcare looks shitty all the time, and private insurance overshadows their medical and administrative fuck ups with celebrity spokespeople, sound design, puppies, and talks about bare-minimum services like insurance companies are benevolent and care, of course, health insurance-funded private medical systems look better. Health insurance is the biggest racket since self-check-out at the supermarket. Self-service checkout makes as much sense as paying someone else to gleefully paint their fence.
It’s simple. If we don’t fund government services like veterans’ healthcare, they don’t work. Unelected douche canoes like Grover Norquist want the government to fail and benefit their own personal gain. They actually brag about it. I don’t want someone fixing my car who hates cars. Things like this inhibit progress. Could you imagine if the stagecoach industry blocked progress in automobiles the way fossil fuel interests have tried to kill electric cars? Sure, it would create jobs for horse shit removal, but it still would stink.
Good Government Is Possible
In that poorly named but well-crafted BBB bill, there were some great changes for all American citizens regarding healthcare infrastructure, especially for veterans. But of course, a small majority in the Senate removed that. Elected officials who are supported by pharma and health insurance companies can’t make government-funded healthcare look like a good option to voters.
What if VA hospitals were not 50 years behind in improvements? What if there was an updated system for medicare that made getting treatment less financially painful? What if veterans everywhere got better healthcare? No way. If government services like Veterans Healthcare and Medicare are properly funded, how would Americans continue to remain divided thus continuing to vote against our own best interests?
You Have The Power to Help Change This
Next time you think about thanking me for my service, don’t. Thank me by voting for representatives who will legislate for veterans in good faith by funding veterans services over privatization. It will work. I’m exhausted, and it would be great if I didn’t have to fight for simple treatments that when denied kneecap my quality of life and cost taxpayers more money in the long run. If you want government services to work properly, especially for veterans, stop trying to make government so small it can be drowned. The only difference between the quality of Kaiser Permanente and VA Healthcare is their PR budgets.
NOTES AND REFERENCES
*The real names of professionals in healthcare in all of my posts have been changed for privacy and to assert the humanity of those who work as public servants and private company employees.
I created a healthcare category. Veterans’ healthcare & insurance-funded health care have a lot in common, so Voila! It’s all in one place.
I’m a 100% service-connected veteran of nearly 30 years. I have advocated for myself as both a veteran and private insurance-funded healthcare*.
The only difference is that one healthcare system can pass laws to prevent treatment, and the other lobbies politicians to pass laws to deny services to their customers.
My goal is to share my experiences to promote more questions that will inspire Americans to ask a minimum of one of these three:
1. Why isn’t veterans’ healthcare adequately funded?
2. Veterans have family and friends who die from inadequate health care*. Why aren’t all Americans getting the medical care and social services we need?
3. How is someone with no medical training in diagnostic medicine paid to deny needed health care and treatments based on the best bargain in favor of insurance company profits?
References
Grammarist, “Healthcare vs Health Care“*