Well, I’ve finally gotten the help I need.
The Mighty Turtle Podcast was tough to manage all on my own, so I reached out to friends at Jo-Kers Productions and developed the show. My podcast is called The Karen Vasquez Show. At first, I felt a little weird naming it after me, but it’s alot easier to remember than scleroderma.
Here’s the format: Each show begins with a short discussion about my experience with scleroderma and then a guest comes on to talk about anything and everything.
I will begin blogging again, but before I do I will be recording podcast episodes and filming more Scleroderma in 60 Seconds videos. Please join me at my new social media handle, @thekarenvasquezshow on Instagram and the new show on Substack and soon on Apple Podcasts.
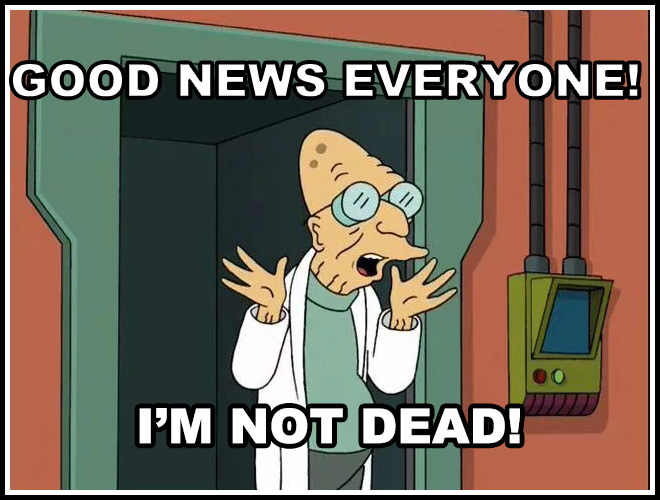
My goal is still the same, to raise awareness that scleroderma or any chronic illness diagnosis is not a death sentance and teach people by laughing at what scares me.
As always, I a grateful for your continuous support.
Yes, that is a toothbrush in the photo. I’ll explain that in another post. It’s what the kids call an Easter egg.
My overall thesis for my blog has always been that we have more in common than we think, like with cancer and scleroderma. Autoimmune illnesses like scleroderma, and cancer are completely different illnesses; but both used to be death sentences. Many cancer drugs, like methotrexate, are used off-label, improving the lives of countless patients with autoimmune diseases. I am one of those patients.
Methotrexate slows the growth of tumors, cures deadly pregnancy complications like ectopic pregnancies, and slows the progression of deadly autoimmune diseases. Methotrexate has a wider range than Mariah Carey.
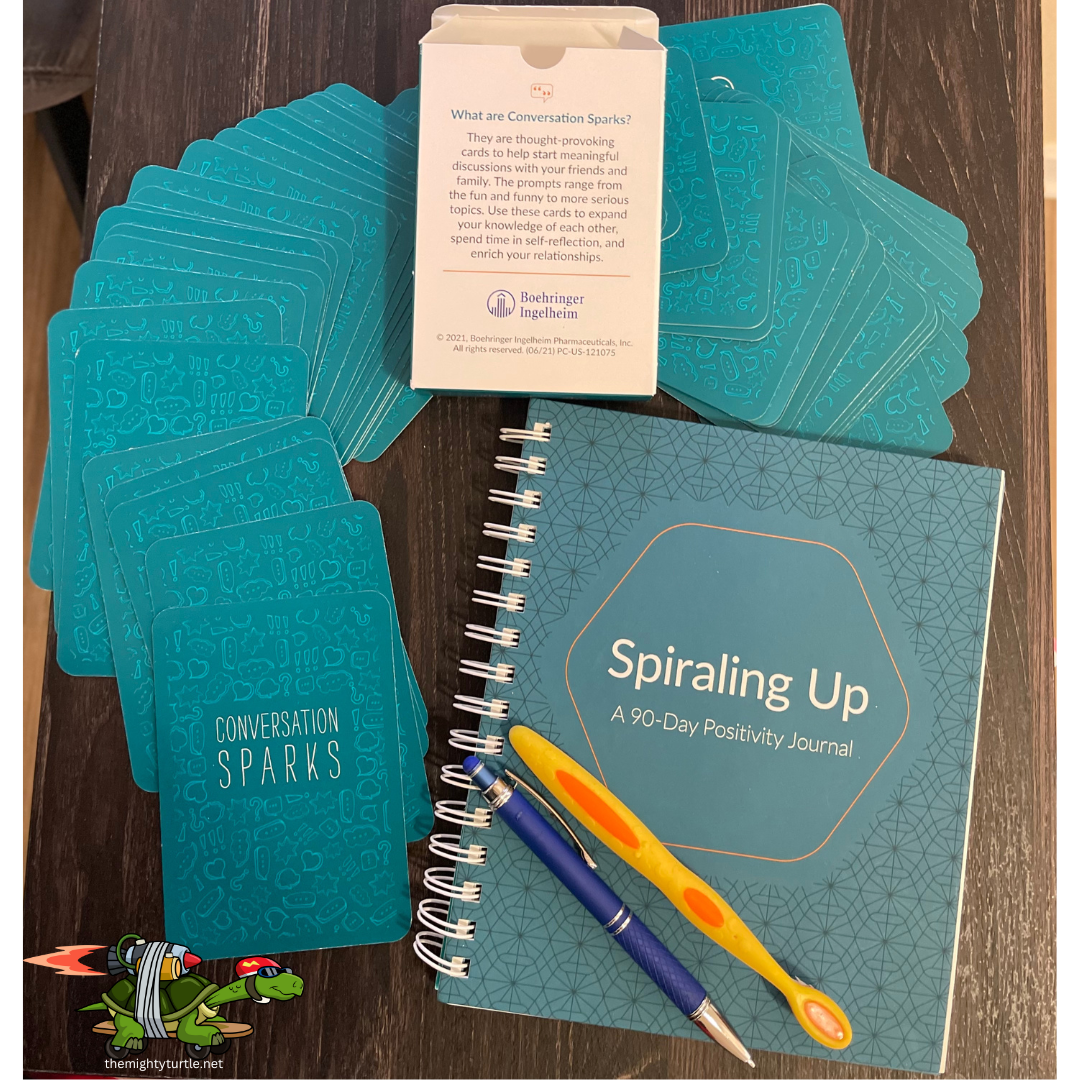
Methotrexate isn’t the only drug that can be used for autoimmune illnesses. I was prescribed Ofev in 2022. Ofev is a lung cancer drug now approved by the FDA to treat pulmonary fibrosis. I’ve taken a lot of medications for scleroderma, but this cancer drug is the first to send me games and a journal. Ofev has a program called Open Doors. It’s a patient support program.
I went to Ofev’s website and filled out some online forms. A nurse from Open Doors contacted me. The nurse’s job was to ensure I understood what I was being treated for, and the side effects of my treatment. I was given phone numbers and was told I would be sent some things to help me communicate with my friends and family.
Of course, I will always talk to my doctors and pharmacists first about my treatment. Open Doors does not replace my doctor and pharmacists who manage me directly. This is for information about dealing with side effects and questions about the drug and tracking my reactions to treatment, and oh the schwag!
Remember the Big Pharma schwag from the 1990s? They had the best pens and stress balls. But this time, instead of pens, I was sent a deck of cards with conversation prompts, a journal with positive writing prompts, and material about managing side effects. This is the first time a pharmaceutical company has sent me something helpful to cope with the side effects and provide a source for questions about Ofev itself, and now I have a ton of writing prompts.
I love writing prompts, especially when it comes to writing about my experience. If you’ve read my blog before, you’ve seen that I tie things together. Sometimes I take the whole hayride to get to my point, and writing prompts make the hay ride shorter.
I’ve challenged myself to use the cards to write something once daily for thirty days. I won’t be posting my daily posts from these prompts to leave myself the option to write about “wounds” in this exercise. “Scars” are former “wounds” that have been processed in therapy that I’m comfortable talking about. I’m going to use the hell out of writing prompts.
References
Methotrexate History
Methotrexate in Rheumatoid Arthritis (2013)cancer,
In this episode of scleroderma in 60 seconds, I share what I do to fight hair loss due to medication or product build-up. Like all episodes, this is helpful to chronic illness patients with conditions like scleroderma and anyone combating a loss like hair due to product build-up and/or their medication. We all have more in common than we think.

Both calcinosis and a typhoon look calm from above, but below, it’s a real shitshow.
Yesterday, I discovered the podcast service I had archived my podcast, so The Mighty Turtle podcast has moved. It will be in Apple Podcasts in a few days, but if you’d like to check out the reposted episode one, check it out HERE.
I’m still recovering from calcinosis from hell, which I address later in this post. I originally started this blog in 2012, but I had to move it and instead of reposting, I’m going through my posts from the past 11 years. My original blog posts were too long and all over the place. It’s taken graduate school and lots of therapy to help me understand how to tell a story without launching myself in an entirely different direction from my point. So instead of reposting them here, I will just chop them up and revise them and post them. If you’re into self-punishment or need help falling asleep, you can see some of my old posts Here.
About my calcinosis wound on my right leg; I feel like I have a handle on it, but I’ve been out of circulation for almost a year. It began with a lump on my right leg. I had it a while after I banged my shin on an open dishwasher door in 2018. Thanks to “The Rule of Ouch”- that’s where the sight of an injury or wound is repeatedly banged in the same place. When an impact happens over and over, antibodies are deployed by our immune system which in my case kills some healthy cells. Where do those dead cells go? If they are not broken down, they accumulate. The lump on my leg was an accumulation of cells in their final state, calcium.
Don’t let the name Calcinosis fool you. It has nothing to do with our calcium intake or diet. Calcium is the final state of living cells. I learned that from a podcast about aquamation, in addition to what doctors have told me.
This calcinosis wound from hell on my leg has been open since March of 2021. (Yes, I feel dizzy just thinking about it.) Luckily, I’ve had enough of these overwhelming wounds that would make the toughest person cry, tell all the secrets and beg for their mommy. So as angry as I was about having to sit still, I knew that these wounds would heal and I’d be out and about soon. And now, after pushing these calcium rocks out of my leg, they are gone, and my wound is finally closing. That’s right, I’ve been pushing rocks out of my leg for over fifteen months and counting.
Unfortunately, these rocks were ugly so I couldn’t make jewelry. (I saw something like that in the Beck episodes of Futurama.). It also meant not only did I have to avoid standing or walking, but I also have to elevate my leg constantly to keep the swelling down. I found the more active I was, the longer it took to close. I have reached the part of my recovery where my wound is almost closed, so I’m easing back into action, slowly.
I am hoping my lack of activity and weekly wound care appointments will continue to speed healing. Right now, I’m doing a lot of stretching yoga, with some great mobility exercises taught by Rachel Lando. She’s also the guest on the first episode of my podcast. She was going to cohost, but she’s super busy teaching fantastic yoga and she will definitely be back as a guest.
Right now, I’m doing 20 minutes at a time at my computer desk. It’s not impossible for me to work from bed, but it does a number on my back, so I’m not doing that. It does make me a million times slower.
Sometimes, I feel the need to talk about why I write this blog and do stand-up comedy about scleroderma. It’s never my only topic, but it’s always there. We all contribute to the scleroderma fight no matter how little we think we are doing. Sometimes, just being a patient is all we can contribute and that’s always enough. Simply staying alive helps scleroderma patients who come after us because doctors talk to each other. I learned that when my son was born.
When we met my son’s pediatrician and told her how my son came into the world two months early, she said, “Oh, that was you? I heard about your case.”
It made me happy for two reasons:
1. Doctors discuss difficult cases within their community.
2. She knew what she was dealing with regarding the care of my son.
Even after medical school, medical providers continue to learn and teach others. Doctors talk about difficult cases with their peers and I never miss a chance to work with a medical student.
I’ve met doctors in random settings who worked with me as medical students. I’m surprised and flattered they remember me. I’m sharing it here because I didn’t know it at the time, but I’ve been raising scleroderma awareness and teaching doctors to listen to chronically ill patients for decades. Actually, we all do.
It would be amazing to walk into a hospital for care and have a medical staff that knows exactly what to do for my scleroderma symptoms and complications, but that’s a fantasy. In the real world, medicine is a practice, and not every clinician knows a lot about scleroderma.
And how could they? There are over eighty types of autoimmune diseases with intersecting symptoms and complications. And no matter what chronic illness we have, in addition to the specialist for that chronic condition we must have a team of specialists for our systems because let’s face it, it’s fucking complicated.
This doesn’t mean that I believe more about scleroderma shouldn’t be taught in medical school. It means that I am aware of the fact that scleroderma is one of the thousands of conditions and chronic illnesses that are out there. So when given the opportunity to teach, I say yes.
When offered the chance to work with medical students, I always say yes. It’s the easiest way to raise scleroderma awareness. Sometimes, medical students will just observe. Sometimes they’ll ask questions with their attendings present, and sometimes they’ll come in to practice asking patients questions for patient assessment.
There have been times in the hospital when I don’t feel up to talking and students are respectful about it. And maybe talking to medical students isn’t your thing and that’s great. You do you, Boo;-) My point is, that when we do what we are capable of doing, that is enough.
It’s hard to find a silver lining with a chronic illness. Here’s mine.
When we work to stay as healthy as possible or fight the good fight when necessary; we are not only helping ourselves to live longer, more fulfilling lives. We’re also helping scleroderma patients who come after us. We are proving that scleroderma is not a death sentence. We are proving that life isn’t over with a diagnosis. It feels like it, but it’s not.
Also, the nurses and doctors who treat us learn about scleroderma patients. The next scleroderma patient they treat will receive better care because of what they learned from us, even if all we did was receive treatment.
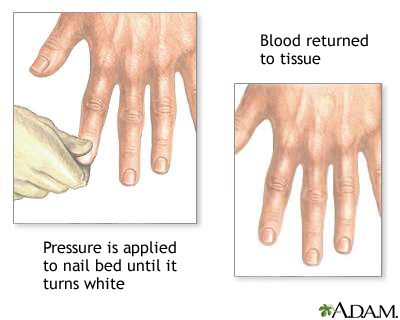
I don’t really remember my first Raynauds attack, but I remember the first time I saw it happen. In 1993, during the last year of my enlistment in the Navy, I had shore duty. Four nights a week, I attended EMT school at Miramar College. I was a “patient” for someone to practice leg splinting. After splinting, blood flow is checked by something called capillary refill.
Capillary refill tests the speed of blood return to a spot on our bodies- usually fingers and toes. When pinched, blood will disappear but should immediately return. In my case, my toenail remained white longer than it should have. Slow blood return is a symptom that indicates something is wrong. My big toe had a slow blood return and while the student EMT was checking the device, my toe turned blue.
The instructor came by to help us troubleshoot. She asked if I was diabetic. I was not. She advised me to get it checked. What she didn’t know is that I had been experiencing numbness and tingling in my fingers and toes with the smallest temperature drop for a little over a year.
I had already been seen by two rheumatologists at Balboa Navy Hospital and my blood tests were inconclusive. I was advised to stop smoking and stop taking birth control pills. I quit smoking and stopped taking the pill, but it kept happening When I followed up with my rheumatologists, they said it was probably nothing and just the way my body works.
The following October, I was seated on the examination table at the Madison Wisconsin Veterans Hospital. Two more rheumatologists were examining me. They looked through a jeweler’s loop just like the rheumatologists at Balboa did, but this time they had an immediate answer; scleroderma.
I was stunned. I had never heard of scleroderma, and neither did my boyfriend who drove me to the doctor that day. My first question was, “Will it kill me?”
Other than the name of my diagnosis, the rheumatologists had very little information about scleroderma and how it would effect me. I was told it could kill me in three years, or I could live to be one hundred.
My boyfriend said that I shouldn’t be consumed by whether or not scleroderma killing me, because I could waste all of my time worrying and end up getting killed by a bus instead. Great, not I’m scared of scleroderma and buses. But kidding aside, he had a point. Nothing had changed since walking into the doctor’s office, except I had a name for what was causing my fingers and toes to turn blue.
Twenty-seven years later, I am grateful to my ex-boyfriend for that perspective. It shaped my way of thinking more than I could’ve imagined back then. My only regret about that day is that I didn’t ask, “Can I drink with these meds?”