In this episode of scleroderma in 60 seconds, I share what I do to fight hair loss due to medication or product build-up. Like all episodes, this is helpful to chronic illness patients with conditions like scleroderma and anyone combating a loss like hair due to product build-up and/or their medication. We all have more in common than we think.

Both calcinosis and a typhoon look calm from above, but below, it’s a real shitshow.
Yesterday, I discovered the podcast service I had archived my podcast, so The Mighty Turtle podcast has moved. It will be in Apple Podcasts in a few days, but if you’d like to check out the reposted episode one, check it out HERE.
I’m still recovering from calcinosis from hell, which I address later in this post. I originally started this blog in 2012, but I had to move it and instead of reposting, I’m going through my posts from the past 11 years. My original blog posts were too long and all over the place. It’s taken graduate school and lots of therapy to help me understand how to tell a story without launching myself in an entirely different direction from my point. So instead of reposting them here, I will just chop them up and revise them and post them. If you’re into self-punishment or need help falling asleep, you can see some of my old posts Here.
About my calcinosis wound on my right leg; I feel like I have a handle on it, but I’ve been out of circulation for almost a year. It began with a lump on my right leg. I had it a while after I banged my shin on an open dishwasher door in 2018. Thanks to “The Rule of Ouch”- that’s where the sight of an injury or wound is repeatedly banged in the same place. When an impact happens over and over, antibodies are deployed by our immune system which in my case kills some healthy cells. Where do those dead cells go? If they are not broken down, they accumulate. The lump on my leg was an accumulation of cells in their final state, calcium.
Don’t let the name Calcinosis fool you. It has nothing to do with our calcium intake or diet. Calcium is the final state of living cells. I learned that from a podcast about aquamation, in addition to what doctors have told me.
This calcinosis wound from hell on my leg has been open since March of 2021. (Yes, I feel dizzy just thinking about it.) Luckily, I’ve had enough of these overwhelming wounds that would make the toughest person cry, tell all the secrets and beg for their mommy. So as angry as I was about having to sit still, I knew that these wounds would heal and I’d be out and about soon. And now, after pushing these calcium rocks out of my leg, they are gone, and my wound is finally closing. That’s right, I’ve been pushing rocks out of my leg for over fifteen months and counting.
Unfortunately, these rocks were ugly so I couldn’t make jewelry. (I saw something like that in the Beck episodes of Futurama.). It also meant not only did I have to avoid standing or walking, but I also have to elevate my leg constantly to keep the swelling down. I found the more active I was, the longer it took to close. I have reached the part of my recovery where my wound is almost closed, so I’m easing back into action, slowly.
I am hoping my lack of activity and weekly wound care appointments will continue to speed healing. Right now, I’m doing a lot of stretching yoga, with some great mobility exercises taught by Rachel Lando. She’s also the guest on the first episode of my podcast. She was going to cohost, but she’s super busy teaching fantastic yoga and she will definitely be back as a guest.
Right now, I’m doing 20 minutes at a time at my computer desk. It’s not impossible for me to work from bed, but it does a number on my back, so I’m not doing that. It does make me a million times slower.
Sometimes, I feel the need to talk about why I write this blog and do stand-up comedy about scleroderma. It’s never my only topic, but it’s always there. We all contribute to the scleroderma fight no matter how little we think we are doing. Sometimes, just being a patient is all we can contribute and that’s always enough. Simply staying alive helps scleroderma patients who come after us because doctors talk to each other. I learned that when my son was born.
When we met my son’s pediatrician and told her how my son came into the world two months early, she said, “Oh, that was you? I heard about your case.”
It made me happy for two reasons:
1. Doctors discuss difficult cases within their community.
2. She knew what she was dealing with regarding the care of my son.
Even after medical school, medical providers continue to learn and teach others. Doctors talk about difficult cases with their peers and I never miss a chance to work with a medical student.
I’ve met doctors in random settings who worked with me as medical students. I’m surprised and flattered they remember me. I’m sharing it here because I didn’t know it at the time, but I’ve been raising scleroderma awareness and teaching doctors to listen to chronically ill patients for decades. Actually, we all do.
It would be amazing to walk into a hospital for care and have a medical staff that knows exactly what to do for my scleroderma symptoms and complications, but that’s a fantasy. In the real world, medicine is a practice, and not every clinician knows a lot about scleroderma.
And how could they? There are over eighty types of autoimmune diseases with intersecting symptoms and complications. And no matter what chronic illness we have, in addition to the specialist for that chronic condition we must have a team of specialists for our systems because let’s face it, it’s fucking complicated.
This doesn’t mean that I believe more about scleroderma shouldn’t be taught in medical school. It means that I am aware of the fact that scleroderma is one of the thousands of conditions and chronic illnesses that are out there. So when given the opportunity to teach, I say yes.
When offered the chance to work with medical students, I always say yes. It’s the easiest way to raise scleroderma awareness. Sometimes, medical students will just observe. Sometimes they’ll ask questions with their attendings present, and sometimes they’ll come in to practice asking patients questions for patient assessment.
There have been times in the hospital when I don’t feel up to talking and students are respectful about it. And maybe talking to medical students isn’t your thing and that’s great. You do you, Boo;-) My point is, that when we do what we are capable of doing, that is enough.
It’s hard to find a silver lining with a chronic illness. Here’s mine.
When we work to stay as healthy as possible or fight the good fight when necessary; we are not only helping ourselves to live longer, more fulfilling lives. We’re also helping scleroderma patients who come after us. We are proving that scleroderma is not a death sentence. We are proving that life isn’t over with a diagnosis. It feels like it, but it’s not.
Also, the nurses and doctors who treat us learn about scleroderma patients. The next scleroderma patient they treat will receive better care because of what they learned from us, even if all we did was receive treatment.
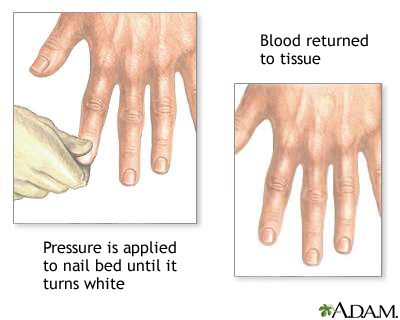
I don’t really remember my first Raynauds attack, but I remember the first time I saw it happen. In 1993, during the last year of my enlistment in the Navy, I had shore duty. Four nights a week, I attended EMT school at Miramar College. I was a “patient” for someone to practice leg splinting. After splinting, blood flow is checked by something called capillary refill.
Capillary refill tests the speed of blood return to a spot on our bodies- usually fingers and toes. When pinched, blood will disappear but should immediately return. In my case, my toenail remained white longer than it should have. Slow blood return is a symptom that indicates something is wrong. My big toe had a slow blood return and while the student EMT was checking the device, my toe turned blue.
The instructor came by to help us troubleshoot. She asked if I was diabetic. I was not. She advised me to get it checked. What she didn’t know is that I had been experiencing numbness and tingling in my fingers and toes with the smallest temperature drop for a little over a year.
I had already been seen by two rheumatologists at Balboa Navy Hospital and my blood tests were inconclusive. I was advised to stop smoking and stop taking birth control pills. I quit smoking and stopped taking the pill, but it kept happening When I followed up with my rheumatologists, they said it was probably nothing and just the way my body works.
The following October, I was seated on the examination table at the Madison Wisconsin Veterans Hospital. Two more rheumatologists were examining me. They looked through a jeweler’s loop just like the rheumatologists at Balboa did, but this time they had an immediate answer; scleroderma.
I was stunned. I had never heard of scleroderma, and neither did my boyfriend who drove me to the doctor that day. My first question was, “Will it kill me?”
Other than the name of my diagnosis, the rheumatologists had very little information about scleroderma and how it would effect me. I was told it could kill me in three years, or I could live to be one hundred.
My boyfriend said that I shouldn’t be consumed by whether or not scleroderma killing me, because I could waste all of my time worrying and end up getting killed by a bus instead. Great, not I’m scared of scleroderma and buses. But kidding aside, he had a point. Nothing had changed since walking into the doctor’s office, except I had a name for what was causing my fingers and toes to turn blue.
Twenty-seven years later, I am grateful to my ex-boyfriend for that perspective. It shaped my way of thinking more than I could’ve imagined back then. My only regret about that day is that I didn’t ask, “Can I drink with these meds?”



Hello! So…someone from a private healthcare referral service received someone else’s death notification from the VA, then reached out to Angela*, my home occupational therapy provider, and told her I had died. The good news is, I’m not dead. Like all my posts, this is another story about my personal experience that I hope will make us all better health care advocates for ourselves and others.
The VA Did Not Fuck Up
Whenever I talk about a medical mistake, it’s usually assumed that it’s a mistake by Veterans Healthcare. The VA did set me up with OT, but they did not call and notify anyone that I was dead. The VA informed Bob, an employee of a government contractor that refers VA patients to private health care providers about a death. Bob mistakenly thought the decedent was me.
How Did I Get Here? Dancing.
During a hospital stay in December 2021, Madison, my in-patient social worker concluded that I needed ongoing home occupational therapy. Madison had to send that referral to another department to determine if I am entitled to home occupational therapy. Once approved, my referral was sent to Bob’s referral service to connect me with an OT provider.
The provider sent a patient treatment manager, an OT named Emma, to determine the course of my treatment. Emma submitted the treatment plan, then another OT named Angela performed my treatment. In my case, I was approved for 10 visits, with a treatment plan of two visits per week, to be reassessed by Emma after all 10 visits.
I was frustrated that I would have to be reassessed every five weeks to determine that I had not somehow been miraculously cured. Through the years, I’ve had different partners but it’s always the same dance. Before I knew the dance, most practitioners dismissed my request for any type of preventive therapy for scleroderma. Before it became the public norm to encourage people with disabilities due to chronic illness to stay active, any occupational therapy to slow down the progression was considered a waste of money. It took a long time for me to find medical providers who would help and encourage me to live a fulfilling life that met my standards.
More for Context
It’s not that I would need OT twice a week forever. My goal is always to get to a spot where I need fewer visits. Why do I think that’s helpful? That’s how it was done in the second half of the 1990s for me through the Madison Wisconsin Veterans Healthcare System. Ever hear the phrase, “If you’ve ever been to one VA hospital, you’ve been to only one VA hospital”? It’s fucking mind-numbing how each state can have different policies for its VA healthcare system.
When I lived in LaCrosse, Wisconsin, I was allowed weekly occupational therapy at a private facility. Back then it was called Fee Basis, and it was god damn spectacular.
When I returned to California in 1999, I presented Debbie, the occupational therapist at the San Diego VA, my treatment plan from the Madison VA hospital in Wisconsin. Debbie determined that the cost of local OT therapy was a waste of government funds to delay the inevitable. San Diego and Loma Linda VA Healthcare System felt the same way. Now, I’m at the West LA VA and after fighting for decades, I’ve got the OT I need. Well, I did until my case was closed thanks to the death fuck-up.
Treatment Interrupted
When any kind of treatment or therapy suddenly stops, it sets me back in function and reduces the odds of my fingers recovering as well as they could have. It’s a domino effect. I subconsciously guard an injured spot only to become aware of it after getting an additional impact wound because I zigged when I should’ve zagged. Those injuries are painful and protecting wounds by compensating in other ways leads to additional injuries and infections. Once this domino effect is in motion, it’s as easy to handle as nailing Jello to a tree.
How I Dropped Off the Radar This Time
It’s easy to fall between the cracks when care suddenly stops. Frustration is overwhelming and there’s always a chance of a visit from the Crippling Depression Fairy. It’s happened to me a lot.
Here’s what happened this time. A couple of Fridays ago, my OT therapist Angela, tested positive for COVID. (I tested negative BTW) She had no symptoms, but my visits had to be canceled until Angela was cleared. They couldn’t just send out another because I had been exposed to Covid. A week went by, so I reached out to her via text to see if she had been cleared. That’s how I discovered my death had been reported.
Now, I’m into the second week of no treatment. I have yet to learn if the referral dance I mentioned earlier must start again. It could be one week or two, maybe a month.
So who is to blame? Is it VA Healthcare? Or the companies paid to manage my case? It’s neither and it’s both. This cluster-fuckery is baked into the design of our shoestring healthcare infrastructure. Screw-ups remotely related to VA services make it easy for public opinion to favor private health care over government-funded healthcare like the VA. If funded properly, VA Healthcare could potentially make a good model for universal healthcare or Medicare for all. But we can’t have that. A small percentage of Americans need to collect dividends for their big pharma and health Insurance stock in addition to those “life saving” stock buybacks.
Ever notice that screw-ups at VA hospitals are all over the news, but rarely from our private hospitals? That’s because private health insurance and private hospitals have bigger public relations budgets.
If government-funded healthcare like VA healthcare looks shitty all the time, and private insurance overshadows their medical and administrative fuck ups with celebrity spokespeople, sound design, puppies, and talks about bare-minimum services like insurance companies are benevolent and care, of course, health insurance-funded private medical systems look better. Health insurance is the biggest racket since self-check-out at the supermarket. Self-service checkout makes as much sense as paying someone else to gleefully paint their fence.
It’s simple. If we don’t fund government services like veterans’ healthcare, they don’t work. Unelected douche canoes like Grover Norquist want the government to fail and benefit their own personal gain. They actually brag about it. I don’t want someone fixing my car who hates cars. Things like this inhibit progress. Could you imagine if the stagecoach industry blocked progress in automobiles the way fossil fuel interests have tried to kill electric cars? Sure, it would create jobs for horse shit removal, but it still would stink.
Good Government Is Possible
In that poorly named but well-crafted BBB bill, there were some great changes for all American citizens regarding healthcare infrastructure, especially for veterans. But of course, a small majority in the Senate removed that. Elected officials who are supported by pharma and health insurance companies can’t make government-funded healthcare look like a good option to voters.
What if VA hospitals were not 50 years behind in improvements? What if there was an updated system for medicare that made getting treatment less financially painful? What if veterans everywhere got better healthcare? No way. If government services like Veterans Healthcare and Medicare are properly funded, how would Americans continue to remain divided thus continuing to vote against our own best interests?
You Have The Power to Help Change This
Next time you think about thanking me for my service, don’t. Thank me by voting for representatives who will legislate for veterans in good faith by funding veterans services over privatization. It will work. I’m exhausted, and it would be great if I didn’t have to fight for simple treatments that when denied kneecap my quality of life and cost taxpayers more money in the long run. If you want government services to work properly, especially for veterans, stop trying to make government so small it can be drowned. The only difference between the quality of Kaiser Permanente and VA Healthcare is their PR budgets.
NOTES AND REFERENCES
*The real names of professionals in healthcare in all of my posts have been changed for privacy and to assert the humanity of those who work as public servants and private company employees.
I created a healthcare category. Veterans’ healthcare & insurance-funded health care have a lot in common, so Voila! It’s all in one place.
I’m a 100% service-connected veteran of nearly 30 years. I have advocated for myself as both a veteran and private insurance-funded healthcare*.
The only difference is that one healthcare system can pass laws to prevent treatment, and the other lobbies politicians to pass laws to deny services to their customers.
My goal is to share my experiences to promote more questions that will inspire Americans to ask a minimum of one of these three:
1. Why isn’t veterans’ healthcare adequately funded?
2. Veterans have family and friends who die from inadequate health care*. Why aren’t all Americans getting the medical care and social services we need?
3. How is someone with no medical training in diagnostic medicine paid to deny needed health care and treatments based on the best bargain in favor of insurance company profits?
References
Grammarist, “Healthcare vs Health Care“*

And of course, the Turtle’s name is Ricky-Bobby.
Hello, my name is Karen Vasquez. In 1994 I was diagnosed with a rare progressive degenerative disease called, scleroderma. I felt isolated, even in support groups and after the internet became a thing. I thought no one could possibly understand what I was going through. In 2007, I was diagnosed with sarcoidosis in addition to scleroderma and that opened my eyes to the similar symptoms experienced by people with different chronic illnesses. I started talking to people with other chronic illnesses and people who don’t have an ongoing medical stuggle. I found one thing that connected us all, grief. I may not know exactly how a person with Lupus feels, but I do understand their loss of function and/or abilities.
Not only did I find grieving loss in common with others who had different symptoms and hard to pronounce names, but I also found grieving loss in common with people who did not have chronic illnesses. Sure, I don’t know what suddenly losing a job after twenty-three years feels like, but I do understand what it’s like to lose my thumb at twenty-five years old. Yes, they are distinctly different devastating losses, but both trigger overwhelming grief.
The Grief Connection
In college, I was introduced to two books; one in psychology class and the other in philosophy class. They are The Five Stages of Grief and The Power of Myth. The Five Stages of Grief, by Elisabeth Kübler-Ross, is based on her studies of death and dying. The Power of Myth is based on a six-hour conversation between journalist Bill Moyers, and author of The Hero’s Journey, Joseph Cambell at George Lucas’ Skywalker Ranch in 1998.