Big anniversary today. Two years, the big 02. It’s been two years since I moved. I am even unpacked.
It turns out that moving is not a coping skill.
This year I had pneumonia and then covid. Part of me believes that it’s my body telling me to slow down and an even bigger part tells me I need to use hand sanitizer and masks.
I was all set up to quit comedy and then I booked a local show for tomorrow, Wednesday September 25th. I’m adapting my comedy schedule. I just need to ask to go up early in the show so I can go home to sleep at a decent hour.
I’m now the comedian who insists on going to bed at a decent hour. It may be permanent. I won’t know if I don’t try. I’m challenging myself to stay on my daily routine. Recently Jamie Lee Curtis said that we need more matinees. I’m just putting it out there in the universe.

We all have a friend who starts talking about something and then takes us somewhere we had no idea we were going. It’s me. Hi, I’m Karen. This post is all over the place and I’m taking suggestions.
My goal with the blog and now my podcast- I have yet to update – is to bring chronic illness awareness outside the scleroderma community, but there’s more to it. After twenty-seven years, I finally understand why I am so pissed off about American Healthcare. American Healthcare is the problem.
Since being diagnosed with my second chronic illness, I realized scleroderma was only one of my issues. It’s never just scleroderma.
But first, scleroderma. Like many with chronic illnesses, I felt isolated because I knew no one else with scleroderma when I was diagnosed. I used to get upset when friends and family went to cancer fundraisers, but never my scleroderma walks.
It’s not that they didn’t like me. It’s that scleroderma had never touched their lives on a daily basis like their loved one with cancer or whatever wasn’t scleroderma. So I began to look for things I have in common with other people or illnesses. The one thing I found constant in everyone is that we all face challenges. One challenge is not more valid than another. It’s not a contest. Also, when there are breakthroughs in conditions or diseases other than mine, this elevates care for all.
Everyone knows about cancer. But did you know that cancer medications like Ofev for lung cancer treat pulmonary fibrosis in scleroderma? Do you know how they found out? Because when a drug is developed and approved by the FDA, the research doesn’t stop there. It continues. Things change as more information is studied, and then studies are studied and repeated.
I have pulmonary fibrosis due to scleroderma. The good news is that in the research of medication to treat lung cancer, someone noticed some benefits for individuals with pulmonary fibrosis. Recently, that medication was approved to treat and prevent pulmonary fibrosis with scleroderma by the FDA.
The situation I faced was not unlike what all Americans faced during the COVID vaccine roll-out. Is the benefit worth the risk?
Now, like the covid vaccine, Ofev is relatively new. Both medications were not created overnight. Although it felt like it with the covid vaccine, it was not created overnight. Here’s why: In my case, I had my radar up because I knew that someday my lungs would harden enough for me to need supplemental oxygen or a lung transplant. So when my prescribing physician told me the FDA approved something for pulmonary fibrosis with scleroderma, I wanted it yesterday.
With the Covid vaccine, there were already vaccines available for the viruses like Covid. Once we were able to genetically code it (and by we, I mean researchers doing actual research. not blog comparison), it was tested, approved, and tested more and then approved for the population by the FDA. No one pulled this vaccine out of their ass. Just like no one pulled Ofev out of their ass.
With Ofev, the side effects and complications risks were present, and I had to learn how to manage them so my body could continue to tolerate prolonged use. Was I going to try it, even though it’s relatively new but has been deemed safe by the FDA? Fuck yes. Because I am lucky to have lived long enough to stop the hardening of my lungs.
The risk of side effects and even death, is worth it to avoid more hardening of my lungs. This is an opportunity to keep my lungs functioning without supplemental oxygen or the need for a lung transplant.
So if you come at me with the whole, Covid vaccine is new, and you’re declining your vaccination because some guy with no medical training tells you it’s not studied enough, I will have to tell you to fuck yourself. That’s how medicine works, asshole.
Those who refuse to get vaccinated for anything that benefits public health (if your health allows you to be vaccinated), you put millions of other Americans, including me, at risk of dying. Due to the way medical necessities are handled in the United States, many freedoms are already taken away from disabled and chronically ill Americans.
So we’re restricted by the shitty American healthcare system, and then there are self-righteous anti-vaxxers restricting us even more.
We already receive the bare minimum of assistance that helps us thrive in our community. We are at the mercy of our caregivers, the for-profit companies that pay shareholders instead of staffing best for patients. We are forced to wait for life-sustaining care or given equipment that crates more problems because everything is cost over convenience.
I honestly don’t know my mission for this blog yet. But I know that Americans with disabilities and chronic illnesses are treated like shit here in the United States. And I’m fucking tired of it. Non-profit foundations compete for funds. Every year chronic illness patients have to travel to the capital of our nation and beg our representatives to help us get better research and care. Every time I see it, I admire the struggle these patients have to go through so whatever representative can have a photo opp saying, “See, I do care.” And then the same representatives vote against assistance programs after the photo opp. I am tired of seeing chronic illness patients and disabled Americans struggle needlessly.
I’m trying to figure out a way to show Americans who believe that Social Security and Medicare should be removed. That is a stupid idea. We need to make it better. And recent COLA increases are a start. When someone’s evaluated, it’s like a guilty until proven innocent thing. It isn’t enough to have the diagnosis; we must live at the lowest rung of the economic ladder.
I am lucky. I have veterans benefits in addition to Social Security and Medicare. People have told me that I should get the best because I’m a veteran. But you know, everyone who serves their country knows someone who has to choose between medicine, food, and rent. All Americans deserve the best healthcare. The reason we all don’t have it is because insurance companies can afford to pay lobbyists to keep it that way. It’s probably more complicated, but can we all start thinking about this?
The only suggestion I have right now is to look at who you’re voting for.
Hello! It’s been a while since I’ve posted, and I’ll catch you all up, but first, I see a lot of new readers so here is a little backstory. Those of you returning, welcome back! If you’d like to, skip the backstory, scroll down to Medical Mayhem.
In 1994, I was diagnosed with scleroderma, then in 2007 with sarcoidosis- that’s when I discovered chronic illnesses are just like potato chips: you’re going to have more than one.
After some harrowing infections, hospital stays, and new complications, I learned that if I could live through the worst of a complication, whatever I am going through is worth the fight because of what awaits me on the other side: More time with friends and family.
I have never called my diagnosis terminal. There have been some close calls and a few scares- not all related to my chronic illnesses. There are so many other ways to die.
Through the years, I learned to advocate for myself using humor. It started out by learning to explain scleroderma without making people cry. Today, most people I run into have heard of scleroderma thanks to Bob Saget and his work raising awareness and funds for a cure for the Scleroderma Research Foundation. But back in 1994, most people hadn’t heard of it, and those who did know, only knew of it as a death sentence. I am living proof that better treatments become available with time.
When my hands began to change, people asked more questions. I found that if I could bring in some humor, it kept people focused on what scleroderma was, instead of pitying me. Eventually, I used humor to teach doctors, nurses and anyone whomever would listen, about scleroderma.
I also have a little privilege as a veteran. Most people with scleroderma & sarcoidosis did not serve in the military. I did, and I have some badass benefits. I never have to choose between rent, medication or food like most people on Medicare and Social Security Disability. I have experience with private insurance before and after preexisting conditions were denied care, in addition to Medicare and Veterans healthcare.
I had health insurance from 2000 to 2008, used with my VA benefits. My current care is provided for free, and the rest of my life is through the VA. Now, instead of health insurance, I use Medicare to supplement my veterans care. My scleroderma & sarcoidosis expert is not part of the VA, so I use medicare to see him. He then prescribes medication and treatment. The rheumatologists at the VA and my outside specialists work together as a team.
Every veteran’s hospital is connected to a medical school which makes them teaching hospitals. My VA hospital works with UCLA, and my outside specialist is a UCLA faculty member. So my doctors from the VA have a relationship with my scleroderma specialist.
Medical Mayhem
I have been told many times by people with different experiences than mine that VAs should be privatized or they are not as good as private hospitals. Not every hospital is equal; however, VA healthcare makes as many mistakes as private healthcare.
As far as mistakes, the ONLY difference between VA Healthcare and private healthcare is a public relations budget. Insurance paid facilities with companies like United Healthcare, Kaiser, or Blue Shield, well we’re going to hear more about “thriving” than all of those mishaps and mistakes thanks to a giant advertising and PR budget. So when something goes wrong at the VA, we only hear about that.
Here is how the clinics at my VA are set up: A doctor who is learning a specialty by practicing is called a fellow. Fellowes are supervised by attending physicians, who are practicing physicians and members of UCLA Faculty. Fellowes see the patients, assess them and bring in the attending physician at the end of the appointment.
Every time I work with a new fellow, they assess me. I listen to what they have to say, and if it conflicts with past treatment, I kindly explain to them how my care works.
For example, I met one fellow who would not prescribe opiates to anyone. She was very new to rheumatology. Anyone who’s ever asked for an opioid, knows what it’s like to be viewed as a drug addict. So when I explained how sometimes I need to “reset” my pain levels by taking Norco for one day or two, then add motrin and tylenol and titrate down to zero. In other words, I need a fucking break.
Pain is part of aging. People with chronic illnesses just experience pain at a younger age and at level eleven. Even after explaining I’ve been doing this for 27 years, and it’s in my chart, she still refused to prescribe them. It used to make me very upset, but with time, I learned that when I don’t agree with a fellow, I wait to speak to the attending. I asked the fellow to speak to her attending about it.
I went home from my appointment with Norco. My “secret” is that I have been managing pain for twenty-seven years. I know the value of Tylenol and Motrin, and I know from experience at what pain level I need a break to rest without any pain, and then I’m good. The attending physicians I have been working with for years know this.
I get that being new to a chronic illness and reading that even after twenty-seven years, I would still need to teach doctors about it doesn’t sound very reassuring, but it isn’t to me. I feel like every doctor, nurse, and medical provider I can teach about my issues, will help future scleroderma patients.
There is no cure for most chronic illnesses, but I have benefitted from new treatments exponentially for the last three decades. If someone else is diagnosed with scleroderma today with my symptoms, they will avoid damage and complications I had. I’m no saint, it does suck, but the opportunity to help others with my experience is fulfilling. It helps me power through things and gives me hope that I will continue to lead a long and fulfilling life.
In this episode of scleroderma in 60 seconds, I share what I do to fight hair loss due to medication or product build-up. Like all episodes, this is helpful to chronic illness patients with conditions like scleroderma and anyone combating a loss like hair due to product build-up and/or their medication. We all have more in common than we think.

Both calcinosis and a typhoon look calm from above, but below, it’s a real shitshow.
Yesterday, I discovered the podcast service I had archived my podcast, so The Mighty Turtle podcast has moved. It will be in Apple Podcasts in a few days, but if you’d like to check out the reposted episode one, check it out HERE.
I’m still recovering from calcinosis from hell, which I address later in this post. I originally started this blog in 2012, but I had to move it and instead of reposting, I’m going through my posts from the past 11 years. My original blog posts were too long and all over the place. It’s taken graduate school and lots of therapy to help me understand how to tell a story without launching myself in an entirely different direction from my point. So instead of reposting them here, I will just chop them up and revise them and post them. If you’re into self-punishment or need help falling asleep, you can see some of my old posts Here.
About my calcinosis wound on my right leg; I feel like I have a handle on it, but I’ve been out of circulation for almost a year. It began with a lump on my right leg. I had it a while after I banged my shin on an open dishwasher door in 2018. Thanks to “The Rule of Ouch”- that’s where the sight of an injury or wound is repeatedly banged in the same place. When an impact happens over and over, antibodies are deployed by our immune system which in my case kills some healthy cells. Where do those dead cells go? If they are not broken down, they accumulate. The lump on my leg was an accumulation of cells in their final state, calcium.
Don’t let the name Calcinosis fool you. It has nothing to do with our calcium intake or diet. Calcium is the final state of living cells. I learned that from a podcast about aquamation, in addition to what doctors have told me.
This calcinosis wound from hell on my leg has been open since March of 2021. (Yes, I feel dizzy just thinking about it.) Luckily, I’ve had enough of these overwhelming wounds that would make the toughest person cry, tell all the secrets and beg for their mommy. So as angry as I was about having to sit still, I knew that these wounds would heal and I’d be out and about soon. And now, after pushing these calcium rocks out of my leg, they are gone, and my wound is finally closing. That’s right, I’ve been pushing rocks out of my leg for over fifteen months and counting.
Unfortunately, these rocks were ugly so I couldn’t make jewelry. (I saw something like that in the Beck episodes of Futurama.). It also meant not only did I have to avoid standing or walking, but I also have to elevate my leg constantly to keep the swelling down. I found the more active I was, the longer it took to close. I have reached the part of my recovery where my wound is almost closed, so I’m easing back into action, slowly.
I am hoping my lack of activity and weekly wound care appointments will continue to speed healing. Right now, I’m doing a lot of stretching yoga, with some great mobility exercises taught by Rachel Lando. She’s also the guest on the first episode of my podcast. She was going to cohost, but she’s super busy teaching fantastic yoga and she will definitely be back as a guest.
Right now, I’m doing 20 minutes at a time at my computer desk. It’s not impossible for me to work from bed, but it does a number on my back, so I’m not doing that. It does make me a million times slower.
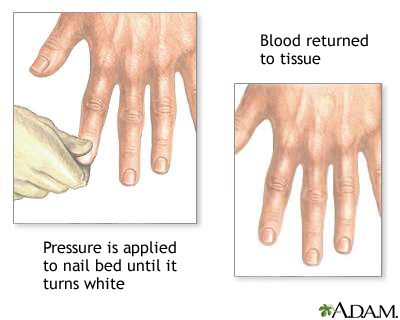
I don’t really remember my first Raynauds attack, but I remember the first time I saw it happen. In 1993, during the last year of my enlistment in the Navy, I had shore duty. Four nights a week, I attended EMT school at Miramar College. I was a “patient” for someone to practice leg splinting. After splinting, blood flow is checked by something called capillary refill.
Capillary refill tests the speed of blood return to a spot on our bodies- usually fingers and toes. When pinched, blood will disappear but should immediately return. In my case, my toenail remained white longer than it should have. Slow blood return is a symptom that indicates something is wrong. My big toe had a slow blood return and while the student EMT was checking the device, my toe turned blue.
The instructor came by to help us troubleshoot. She asked if I was diabetic. I was not. She advised me to get it checked. What she didn’t know is that I had been experiencing numbness and tingling in my fingers and toes with the smallest temperature drop for a little over a year.
I had already been seen by two rheumatologists at Balboa Navy Hospital and my blood tests were inconclusive. I was advised to stop smoking and stop taking birth control pills. I quit smoking and stopped taking the pill, but it kept happening When I followed up with my rheumatologists, they said it was probably nothing and just the way my body works.
The following October, I was seated on the examination table at the Madison Wisconsin Veterans Hospital. Two more rheumatologists were examining me. They looked through a jeweler’s loop just like the rheumatologists at Balboa did, but this time they had an immediate answer; scleroderma.
I was stunned. I had never heard of scleroderma, and neither did my boyfriend who drove me to the doctor that day. My first question was, “Will it kill me?”
Other than the name of my diagnosis, the rheumatologists had very little information about scleroderma and how it would effect me. I was told it could kill me in three years, or I could live to be one hundred.
My boyfriend said that I shouldn’t be consumed by whether or not scleroderma killing me, because I could waste all of my time worrying and end up getting killed by a bus instead. Great, not I’m scared of scleroderma and buses. But kidding aside, he had a point. Nothing had changed since walking into the doctor’s office, except I had a name for what was causing my fingers and toes to turn blue.
Twenty-seven years later, I am grateful to my ex-boyfriend for that perspective. It shaped my way of thinking more than I could’ve imagined back then. My only regret about that day is that I didn’t ask, “Can I drink with these meds?”




And of course, the Turtle’s name is Ricky-Bobby.
Hello, my name is Karen Vasquez. In 1994 I was diagnosed with a rare progressive degenerative disease called, scleroderma. I felt isolated, even in support groups and after the internet became a thing. I thought no one could possibly understand what I was going through. In 2007, I was diagnosed with sarcoidosis in addition to scleroderma and that opened my eyes to the similar symptoms experienced by people with different chronic illnesses. I started talking to people with other chronic illnesses and people who don’t have an ongoing medical stuggle. I found one thing that connected us all, grief. I may not know exactly how a person with Lupus feels, but I do understand their loss of function and/or abilities.
Not only did I find grieving loss in common with others who had different symptoms and hard to pronounce names, but I also found grieving loss in common with people who did not have chronic illnesses. Sure, I don’t know what suddenly losing a job after twenty-three years feels like, but I do understand what it’s like to lose my thumb at twenty-five years old. Yes, they are distinctly different devastating losses, but both trigger overwhelming grief.
The Grief Connection
In college, I was introduced to two books; one in psychology class and the other in philosophy class. They are The Five Stages of Grief and The Power of Myth. The Five Stages of Grief, by Elisabeth Kübler-Ross, is based on her studies of death and dying. The Power of Myth is based on a six-hour conversation between journalist Bill Moyers, and author of The Hero’s Journey, Joseph Cambell at George Lucas’ Skywalker Ranch in 1998.